Dermatoses of Pregnancy, feat. Dr. Laura Hanks
/Here’s the RoshReview Question of the Week!
A 30-year-old G1 woman presents at 34 weeks gestation to the office with severe itching and a rash that suddenly developed across her abdomen starting around her umbilicus. The rash is mostly urticarial papules and plaques, but there are a few scattered bullae. Which of the following is required to confirm the suspected diagnosis?
Check your answer at the links above and get a special deal on RoshReview!
Today we welcome to the podcast Dr. Laura Hanks, who is an Assistant Professor in the Dept. of OB/GYN at the University of Wisconsin - Madison. She was previously in private practice in Olympia, WA, and did her residency training at the University of Rochester in New York.
Dermatoses are a pretty confusing topic — so if you have access to some textbooks through your medical school or residency libraries, Dr. Hanks bookmarked a few good chapters:
Gabbe’s Obstetrics. Normal and Problem Pregnancies. 8th edition. Chapter 56: Skin disease in pregnancy.
Habif’s Clinical Dermatology. Chapter 6: Urticaria, Angioedema and Pruritus.
Creasy and Resnik’s Maternal-Fetal Medicine. 8th edition. Chapter 69: The Skin and Pregnancy.
What are dermatoses?
Dermatoses of pregnancy refers to a group of skin diseases encountered predominantly during pregnancy or immediately postpartum.
In general there is a lack of understanding of the pathogenesis of most of these conditions and therefore a lack of specific diagnostic criteria.
In the podcast, we use a case: 36y G1 at 22 weeks who develops severe pruritus of abdomen, spreading to thighs.
Differential Dx of Dermatoses
Pruritis of pregnancy (pruritis gravidarum)
Reported in 1.5-2% of pregnancies and occurs most frequently over the abdomen.
Usually just pruritus and no rash
Often presents in the 3rd trimester
Intrahepatic Cholestasis of pregnancy
Reversible form of hormonally triggered cholestasis
Runs in families and typically recurs in subsequent pregnancies
Severe pruritus with no primary skin lesions
Pruritus on palms and soles that later becomes more generalized
Itching correlates with elevated serum bile acid levels and sometimes aminotransferases
Bile acids can pass into fetal circulation and cause placental anoxia and cardiac depression which can preclude premature birth, stillbirth, neonatal respiratory distress syndrome, vitamin K deficiency and coagulopathy in the other and newborn.
Polymorphic eruption of pregnancy (PEP) or pruritic urticarial papules and plaques of pregnancy (PUPPPs)
Affects 1 in 130 to 1 in 300 (0.6%) in the US.
This often presents in the 3rd trimester or postpartum with resolution during the postpartum period more commonly in primigravidae pts
Abdominal distension causes damage to the connective tissue that in turn triggers an inflammatory response.
Associated with multiple gestation due to higher levels of progesterone, which has been shown to aggravate the inflammatory process at the tissue level.
Intensely pruritic urticarial rash with erythematous edematous papules and plaques that starts in the abdominal striae and spares the umbilicus. Can include urticarial and sometimes vesicular, purpuric, or targetoid lesions similar to PG or erythema multiforme. Lesions usually spare the palms and soles.
This is a clinical diagnosis with no lab findings and no indication for biopsies. If a biopsy is preformed it will often show a nonspecific perivascular lymphohistiocytic infiltrate +/- eosinophils
There are also no known risks to the fetus.
Impetigo herpetiformis or pustular psoriasis of pregnancy
Often associated with reduced calcium or Vitamin D
Eruption usually during 3rd trimester, most cases resolve postpartum
Characterized by numerous grouped, discrete, sterile pustules at the periphery of erythematous patches
Lesions typically originate on flexures and progress to trunk. Spares face, palms and soles.
Constitutional symptoms can be common including fever, malaise, diarrhea and vomiting with dehydration.
Lab findings include a luekocytosis, elevated erythrocyte sedimentation rate, hypocalcemia and decreased vitamin D levels
Risk of stillbirth and fetal abnormalities secondary to placental insufficiency
Maternal prognosis is very good with early diagnosis and aggressive treatment, however the increased risk of perinatal mortality may persist despite maternal treatment
Diagnosis is based on histopathology that shows typical features of pustular psoriasis. Direct and indirect skin immunofluorescence is negative
Pemphigoid gestationis
Unfortunately sometimes referred to has herpes gestationis, however it is not related to infection by herpesvirus. This synonym was used to refer to the grouped (herpetiform) nature of the blisters, which often are not herpetiform.
It is best to avoid the term herpes gestationis because of the risk for misleading patients and misinformed health care workers; not using the term avoids potentially inappropriate treatments for herpesvirus.
Rate in the US is 1 in 50,000 (0.002%)
Often presents in 2nd or 3rd trimester and sometimes postpartum (25%) with extremely pruritic, urticarial lesions that typically begin on the abdomen and trunk, that commonly involve the umbilicus. These urticarial plaques can then very quickly progress to widespread bullous lesions that may affect palms of hands and soles of feet. There is often a flare at the time of delivery with resolution during the postpartum period.
Lesions can be similar to PUPPs, however PUPPs lesions begin in abdominal striae and spares the umbilicus unlike PG.
Suggested pathogenesis is complement-fixing IgG antibodies and complement C3 react with amniotic epithelium of placental tissues and basement membrane of the skin causing an autoimmune response resulting in tissue damage and blister formation.
Definitive diagnosis is based on biopsies of the lesions that will show skin direct immunofluorescence shows linear deposition of IgG and C3 along basement membrane.
PG recognizes the same antigen as bullous pemphigoid and they do share certain features; however PG itself is confined only to pregnant women and women affected by gestational trophoblastic disease.
Skin histopathology shows a spongiotic epidermis and marked papillary derma edema and an eosinophilic infiltrate
There is an association between PG and Graves, therefore if you have a pt with PG that is an indication to check thyroid function tests
Given the increased risk of small for gestational age infants and preterm delivery, it is recommended to monitor growth US after diagnosis.
Unfortunately, there are risks to the fetus which include being born with lesions that are transient due to passive transfer of IgG1 antibodies, increased risk of SGA, preterm birth and IUFD.
Atopic eruption of pregnancy
This accounts for over 50% of pruritic dermatoses in pregnancy.
Most likely presents in the 1st and 2nd trimester with resolution in the postpartum period. This earlier onset may help distinguish from other dermatoses in pregnancy.
Features of patchy eczema and papular/prurigo lesions that are located on flexural surfaces, neck, chest, and trunk
Serum IgE is elevated
No known risk to the fetus
Prurigo of pregnancy
In the US this occurs in 1 in 300 to 1 in 450 pregnancies
Presents in the 2nd and 3rd trimester
Grouped excoriated or crusted papules over the extensor extremities and occasionally the abdomen
There are no laboratory findings. There may be elevated IgE levels on serologic tests. Previous reports of unfavorable fetal outcomes have not been confirmed.
Pruritic folliculitis of pregnancy or follicular papulopustular eruption
Rare, exact prevalence is unknown (~30 cases reported). Etiology remains unknown
Presents as pruritic follicular erythematous papules and pustules that primarily affect the trunk in the 2nd and 3rd trimester.
Biopsy is usually unhelpful, however histopathology is that of folliculitis. Special stains, skin immunofluorescence and serologies are negative.
There may be an association with decreased birthweight
And don’t forget derm conditions that are not unique to pregnancy!
Allergic contact dermatitis
Drug reaction
Atopic dermatitis or eczema
Erythema multiform
Scabies
Superficial fungal infections
Folliculitis
Urticaria
Vasculitis
Secondary syphilis
Habif’s Clinical Dermatology
In the case, we obtain an H&P —
She began itching on her upper thighs that then spread to her abdomen, chest, back and arms over several days.
She then experienced severe pruritus on the palms of her hands and soles of her feet. She described having to take her shoes off at work and soak them in ice baths and often sleeping with an ice pack between her hands to sooth the itching.
Benadryl did not seem to help neither did OTC steroid creams.
On exam there were numerous pink-salmon colored annula papules and plaques as well as urticaria with scale within umbilicus, flank, thighs and back. On bilateral medial aspects of feet there were pink-red vesicles with petechial border.
What next? Dermatology referral and biopsies.
Biopsy results: Positive linear deposition of IgG and C3 antibodies along the basement membrane, suggestive of pemphigoid gestationis!
Treating Dermatoses
Generally, same treatment principles apply to all of the specific dermatoses of pregnancy.
Milder disease is treated with topical emollients, calamine lotion, cool compresses or baths, and topical corticosteroids.
Topical corticosteroids (e.g., hydrocortisone, triamcinolone) are classified as FDA pregnancy category C drugs in the old system, but they are still widely used during pregnancy when the possible benefits outweigh the risks for minimal percutaneous absorption.
Intrahepatic cholestasis of pregnancy
Ursodeoxycholic acid 15 mg/kg/day daily, BID or TID until delivery
PUPPs
Topical antipruritic medications, topical steroids and oral antihistamines.
In cases of severe pruritis, a short course of oral steroids can be used.
Impetigo herpetiformis
Systemic steroids are first-line with prednisone dose up to 60-80 mg/day
Calcium and vitamin D replacement as needed. Can lead to remission of eruption
Pemphigoid gestationis
The cornerstone for treatment of Pemphigoid gestationis is oral steroids. Therapy should be directed toward suppressing new lesions and relieving intense pruritus.
The majority of patients will respond rapidly to a relatively low-dose of prednisone (20 to 40 mg/day), however the dose may need to be uptitrated according to clinical response as high as 180 mg/day
Prednisone should be tapered slowly once new blister formation is suppressed
~75% of patients will experience resolution or at least improvement in the late 3rd trimester, but b/c PG typically flares at delivery, steroid dose can be increased in anticipation of birth.
Patients at risk for prolonged or chronic PG are often older with higher parity, more widespread lesions and a history of PG in a prior pregnancy.
Atopic eruption of pregnancy
Topical steroids, antihistamines, UVB phototherapy
Prurigo of Pregnancy
Moderately potent topical steroids and oral antihistamines
Short course of oral steroids is rarely required
Pruritic folliculitis of pregnancy
Low-potency or midpotent topical steroids, benzolyl peroxide and UVB.
Ultimately, the patient in our podcast went on to deliver this pregnancy at 38w4d after a cesarean section for fetal indications, without any signs of neonatal blistering (can be seen in 5-10% of babies of mothers with PG!).
The patient ultimately went on to become pregnant a second time, and this time had lesions at 13 weeks. By 25 weeks, prednisone was no longer providing relief!
Treating refractory PG
A number of alternative treatments have been tested, including:
Intravenous immune globulin (IVIG)
Plasmapheresis
Rituximab
Cyclosporine A
Azathioprine
Dapsone and MTX can sometimes be used postpartum
With shared decision making the pt, her MFM and dermatologist elected to proceed with IVIG infusions which were 3 consecutive days every month until the end of pregnancy.
Her symptoms improved but never completely resolved during pregnancy and she continued the prednisone along with IVIG. She had a scheduled repeat c-section at 37w3d with stress-dose steroids given at delivery. She gave birth to a healthy male infant weighing 8lbs 1oz without any lesions.
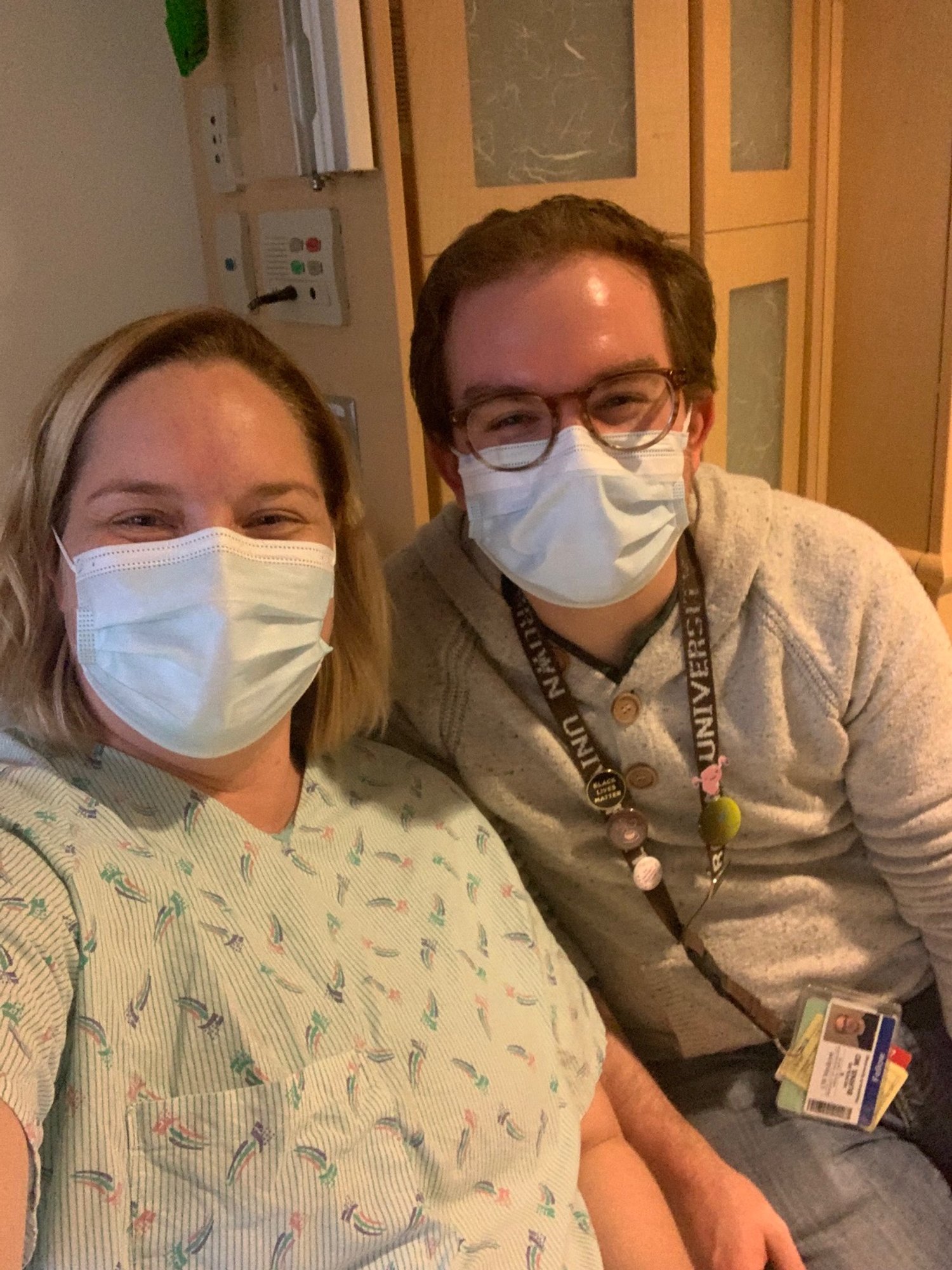
PLOT TWIST! The patient was Laura, and the MFM was Nick!
IVIG Infusions worked once we got them going! ;)