Polyhydramnios
/Reading: SMFM Consult Series: #46: Evaluation and management of polyhydramnios
What is polyhydramnios?
Definition
Abnormal increase in amniotic fluid volume
Using ultrasonography, defined:
Single deepest vertical pocket (DVP) of fluid >/= 8 cm or
Amniotic fluid index (AFI) >/= 24 cm
Prevalence: can complicate 1-2% of singleton gestations, but it is more common in twin gestations, primarily due to complications of monochorionic placentation
Degree of polyhydramnios
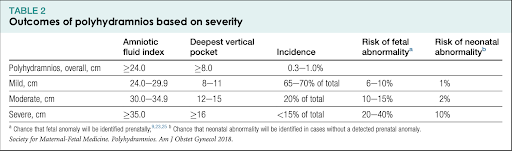
AFI of 24.0-29.9 cm or DVP 8-11 cm = mild (65-70% of cases)
AFI of 30.0-34.9 cm or DVP of 12-15 cm = moderate (20% of cases)
AFI of >/= 35 cm or DVP >/16 cm = severe (<15%)
What causes polyhydramnios, and how do we counsel patients?
Most cases are mild and idiopathic
When etiology is identified, most commonly due to fetal anomaly or maternal diabetes
Most anomalies have to do with swallowing issues
GI obstruction: ie. duodenal atresia, TE fistula, thoracic mass, diaphragmatic hernia
Neuro-muscular: Myotonic dystrophy, arthrogryposis, intracranial anatomy
Craniofacial: cleft lip/palate, micrognathia, neck mass
Fewer due to excess urine production
Renal/urinary - UPJ obstruction, mesoblastic nephroma, Bartter syndrome
Cardiac (basically lesions that lead to high output cardiac failure as well): cardiac structural anomaly, tachyarrhythmia, sacrococcygeal teratoma, chorioangioma
Osmotic diuresis/Other: maternal diabetes, hydrops, idiopathic
What evaluations should be done?
Fetal growth
Fetal cardiac anatomy
Placenta for presence of large chorioangiomas
Fetal movement to assess neurological function
Position of hands/feet ot rule out arthrogryposis syndromes
Presence and size of fetal stomach to r/o tracheoesophageal fistula or esophageal atresia
Anatomy of fetal face/palate
Positioning and appearance of fetal neck to r/o obstructing mass
Fetal kidney to assess for UPJ obstruction
Lower spine and pelvis for evidence of sacrococcygeal teratoma
How worried should the patient be?
Most mild polyhydramnios is idiopathic or due to T2DM, and only 6-10% risk of fetal anomaly, with 1% of neonatal abnormality
However, with severe poly, there is increased risk of fetal anomaly to as high as 20-40% and even risk of neonatal abnormality of 10%
Therefore, those with severe poly should deliver at tertiary care center due to possibility for fetal anomaly
How do we manage polyhydramnios in pregnancy?
Treatment
If the poly is severe enough to cause maternal respiratory compromise, significant discomfort, or preterm labor → this can have underlying etiology
In cases of severe poly that results in maternal respiratory compromise or other discomfort, then amnioreduction can be done
However, the polyhydramnios will usually recur
Indomethacin can decrease fetal urine output
There have been studies looking at women who took indomethacin after amnioreduction to try and decrease reaccumulation and re-amnio
However, preterm infants exposed to indomethacin in utero have decreased neonatal urine output and also elevated serum creatinines
Therefore, indomethacin should not be used for sole purpose of decreasing amniotic fluid in the setting of poly
Antepartum management
Many studies have shown that idiopathic poly has been associated with infant birth weight >4000g in 15-30% of cases
Reports of whether perinatal mortality is increased with idiopathic poly have been inconsistent
Currently recommendation from SMFM is that antenatal fetal surveillance is not required for the sole indication of mild idiopathic poly
Similarly, recommendation is that labor should be allowed to occur spontaneously at term for women with mild idiopathic poly, and that induction, if planned, should not occur at <39 weeks of gestation in the absence of other indications
Most of delivery should be determined based on usual obstetric indications