Placental Pathology I: Basics for the OB/GYN
/Reading: https://www.contemporaryobgyn.net/view/placental-pathology-it-time-get-serious
Great article for this!
What do we hope to get by sending a placenta to pathology?
We want to know what happened!
The goals are to get:
Findings that are relevant to the immediate care of the mother or baby
Findings predictive of possible recurrence that could guide pregnancy care in subsequent pregnancies
Diagnoses that explain adverse pregnancy events (probably the most common reason we send a placenta)
Findings that may be important in medico-legal investigation of perinatal mortality and long-term morbidity
So… which placentas should we send?
There are many reasons, and some of them may depend on your institution, but we have broken this down into three categories
Maternal reasons
Preterm delivery
Unexpected or recurrent pregnancy complications
Maternal systemic disorders (ie. preeclampsia, malignancy, diabetes, etc)
Infection
Excessive third-trimester bleeding
Fetal reasons
Stillbirth, neonatal death
Unexpected NICU admission
SGA or LGA
pH <7.0. 5-minute Apgar <7, or birth depression
Neonatal seizures
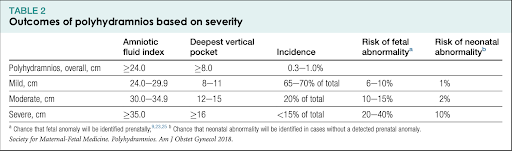
Hydrops, severe oligo/poly
Multiple gestation
Placental reasons
Structural abnormalities or size abnormalities
Possible incomplete placenta
We can see that some of these reasons may not present until after the first day of life, so would recommend holding the placenta for up to 7 days if needed (can be stored unfixed in a fridge for that long!)
The Anatomy and Development of the Placenta
www.placentalab.org
We are going to first discuss a full-term placenta and then go over embryology
The placenta can be thought of as three layers:
Maternal side (basal plate)
Contains trophoblastic cells and decidual cells and contain the decidua basalis
From the basal plate, the placenta septa bulge into the intervillous space, creating a system of grooves
Basal plate is also penetrated by endometrial arteries and venules
Intervillous space - separates the maternal and fetal side
Exchange between the fetal and maternal circulatory systems occur between the main stem villi and the maternal endometrial arteries and venules in this space
Remember: fetal and maternal blood don’t mix!
Fetal side (chorion plate)
Made of connective tissue and contains the amnion, the main stem villi, and chorionic arteries and veins, which then coalesce at the cord insertion site → umbilical cord
The chorionic arteries and veins → arterioles and venules of the main stem villi
The main stem villi project into the intervillous space and are connected to the maternal basal plate by anchoring villi
Placental embryology - super basic
After fertilization and implantation, around day 5, the blastocyst is formed
The blastocyst will eventually implant, and will contain the blastocyst cavity, the inner cell mass, and the trophoblast (which becomes the placenta)
During implantation, there are complex interactions between the endometrium and the embryo → apposition, adhesion, and invasion
Any dysfunction in these 3 processes can lead to abnormal placentation that can lead to affected placental function