Today we’re thrilled to welcome to the show two folks in the #FOAMed #FOAMob space we admire greatly: Dr. Tamandra Morgan, a current PGY-2 in OB/GYN at UCSF; and Dr. Rachel Berell, who did her intern year in OB/GYN at UC-Irvine and is continuing her training in family medicine, with a focus on obstetrics and public health, at Boston Medical Center.
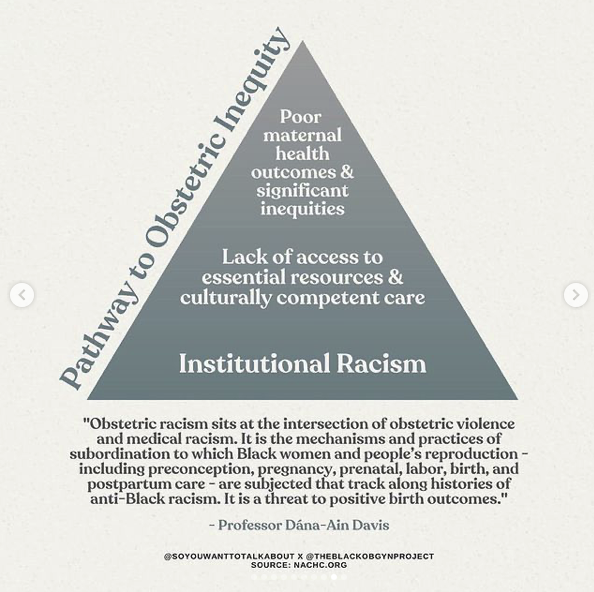
Together, they run the Instagram page @TheBlackObGynProject, which at the time of our recording has 16,700+ followers. They have created this as a space dedicated to educating and promoting anti-racism, equity, and inclusion within OB/GYN, women’s health, and reproductive health care.
We had a lovely interview with them about their work and their experiences.
The Black OB/GYN Project: Learning, Celebrating, Advocating, Healing.
On their Instagram, they have remarkably well-referenced posts about various instances of racism in the history of medicine, as well as how racism and other biases continue to be a factor today.