Surgical Injury, Part I: Bladder Injuries
/Oh no…
Surgical injuries happen in OB/GYN. As you’ve probably shared in your surgical informed consent discussion previously, we often talk about risks like:
Bleeding
Infection
Damage to surrounding structures.
The “surrounding structures” are typically:
Bladder
Most common injury
~0.3% of cesarean deliveries; ~1% of major GYN surgery
Bowel
Less than 1% of GYN surgeries
Ureters
About 0.5% of GYN surgeries
The best prevention for injury is preparation - know your anatomy!
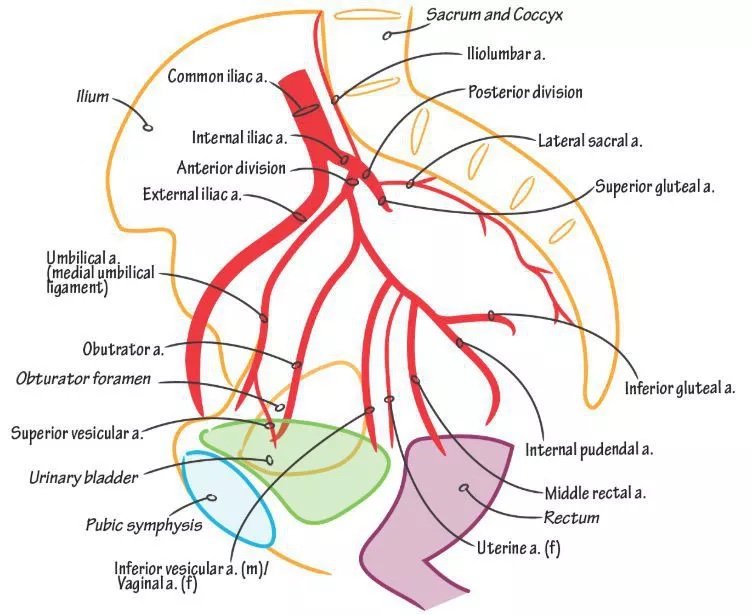
Check out our anatomic meditation on pelvic vasculature.
Look out for future anatomic meditation episodes in the near future!
What are risk factors to intraoperative injury?
Anything that increases surgical complexity, essentially!
More extensive “bigger” surgeries - hysterectomy in particular
Obesity
Age or chronic medical conditions that might limit exposure
Particularly in laparoscopy (i.e., less distension ability)
Emergent surgeries - more frequent bladder injuries in STAT cesareans, 2nd stage arrests
Adhesive disease from prior surgeries, infections, trauma, etc.
Patients with congenital or acquired anatomic differences
Oncology - invasive disease and altered vasculature/structures
What should I do when I identify something that is / may be injured?
If safe to do so: pause and evaluate
Call for assistance: senior colleagues, consultants as needed
If awaiting assistance but need to move on (i.e., bleeding accreta case) – can use “tagging suture” to mark area of concern
Bladder / bowel: place a small, brightly-colored suture (i.e., dyed 2-0 or 3-0 Polysorb/Vicryl) and leave a long tail at the suspected site of injury, so it’s easy to find later on.
Try to identify the mechanism and extent of an injury:
Is it just a serosal tear, or was mucosa exposed?
Were any contaminated (i.e., gastric / intestinal) contents spilled?
Cold cut, or is there potential for thermal (and thus more expansive) injury?
Do I have to deal with this? Can’t I just leave some things unrepaired, and it’ll heal on its own?
In some cases of bladder and bowel injury, very small, non-thermal injuries can be left unrepaired:
Verees needle “clean poke” of small intestine or bladder
However, failure to recognize injury or leaving an injury that is too large or going to expand due to thermal damage unrepaired risks complications:
Early
Copious wound drainage
Abdominal pain - urinary ascites
Fever
Ileus
Peritonitis
Have a high index of suspicion in the postoperative period for a patient having an unrecognized injury, especially if they’re having lots of drainage from the incision or a lot of unexpected pain!
Delayed
Recurrent urinary tract infection
Urinary incontinence
Pelvic pain
Fistula formation
This is of course a major dreaded complication of unrecognized injury.
Quick detour – why can cystotomies occurring in TVT procedures stay unrepaired?
These injuries occur extraperitoneally in the retropubic space.
Simple extraperitoneal injuries almost always heal on their own and can usually just be managed with catheter drainage & won’t form fistula
Injury occurring intraperitoneally should be repaired and are at risk for fistula formation.
We’ve provided the two “windows” of injury for fistulas to form at the time of a hysterectomy with the opening to the vagina:
Vesico-vaginal (bladder-to-vagina, at hysterectomy)
Uretero-vaginal (ureter-to-vagina, at hysterectomy)
Entero-vaginal (bowel-to-vagina)
Bladder Injuries
Site and extent of injury
Most commonly, injuries occur to the dome of the bladder - makes sense anatomically.
Rarely, injuries can occur lower, into the trigone or base of the bladder - this is a danger zone for ureteral injury as well.
Always evaluate the extent of the injury - if limited to the dome, repair is usually possible without consultative assistance. If more extensive or unsure, urology should be notified.
You can use your cystotomy to look into the bladder and see relative anatomy –
ie, visualize the foley, visualize the ureteral openings from above.
If you’re within the dome vs the trigone
If you’re within just a few centimeters of the ureteral openings… may be worth having a consult come by for repair assistance!
Technique of repair for dome injuries
Two layers with absorbable suture – typically use a 2-0 or 3-0.
Don’t use non-absorbable or very delayed absorbable – there will be suture material in the bladder, which acts as a nidus for infection.
First layer: mucosal closure, in a simple running fashion (but not locking).
Second layer: imbricating layer over serosa/muscularis, not entering mucosa (to limit amount of material in bladder).
After repair, check integrity of the bladder repair while you still have access to the abdomen:
A variety of materials can be used to backfill, but generally you want something that is going to have color so you can see a leak, if it’s present.
Sterile milk/formula – works! Though can make your cystoscopy quite cloudy later.
Crystalloid with methylene blue/indigo carmine/fluorescein added.
Many folks may choose to perform cystoscopy at the same time or after backfilling.
The cystoscopy is more for checking your ureteral patency – you’ll have a hard time determining bladder repair integrity from a cystoscopy view unless there’s a large defect.
That said, if your injury was in the dome and far away from ureters, and you could see the ureters from above, cystoscopy may not totally be necessary - as they’re unlikely to get kinked in your repair.
Postop, the Foley needs to stay in place usually 7-14 days.
A void trial and a voiding cystogram should be performed to again demonstrate bladder repair integrity.
Technique of repair for trigone injuries
You should call urology / urogynecology for these.
You will need to assess the status of the ureters, as the ureteral orifices coming into the trigone may be damaged.
IV methylene blue, indigo carmine, or fluorescein along with small dose of furosemide.
If you see dye entering the bladder but not entering the retroperitoneal or intraabdominal space - likely no ureter injury.
Urologists on consultation with a trigone injury may go ahead and place stents to evaluate the ureters.
Placing the stents (and the relative ease or not of doing so) may help them to triage where a ureteral injury is at, and then with repairing the injury ensure the ureter is not incorporated.
Stents may remain in place postoperatively to keep ureters patent, as nearby tissue may swell and obstruct them otherwise.